I’m really excited to finally be able to shout about the new Wellbeing after Miscarriage programme from Tommy’s. This has been a project almost a year in the making and one that will hopefully help to fill a glaring gap in miscarriage support and preparing for pregnancy after loss. I managed all the content development,…
Author: Clare Foster
New content for Sue Ryder – supporting a child when someone is dying
Just a quick update to share that a couple of new content pieces I wrote for Sue Ryder are now live. A further piece on understanding complicated grief is on the way too. Supporting a child when some is dying This is available here. Telling a child someone is dying This is available here.
Action on Postpartum Psychosis’ latest project – peer support for bereavement
Developing peer support for families bereaved by postpartum psychosis On 23rd June 2024, I led APP’s first training day for bereavement peer support volunteers at the Barberry National Centre for Mental Health in Birmingham. We were joined by five new volunteers who want to use their experiences to help support other families who have lost family…
Induction of labour – meeting the needs identified in PIF’s ‘Maternity Decisions: Induction’ survey
A need for better quality, evidence-based, data-led information The results of the Patient Information Forum (PIF) Maternity Decisions: Induction survey in 2021 were not unexpected but made for sobering reading all the same. Rates of induction in the UK are rising, but some women ranked fear of induction as one of their biggest concerns as…
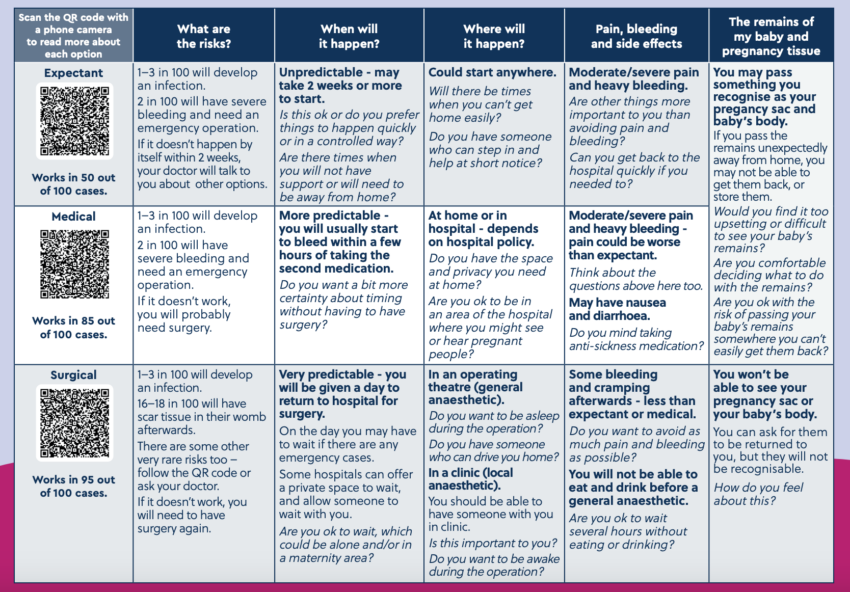
Management of miscarriage – new decision aid
The MifeMiso trial After a missed or incomplete miscarriage, women usually have the option of conservative (natural), medical or surgical management. The MifeMiso trial, published in 2020, showed that taking misoprostol and mifepristone was more effective for the medical management of miscarriage vs. misoprostol alone. In August 2023, NICE guidelines were updated to direct healthcare…
Children who are aged 2-5 when they lose a parent to suicide are most likely to go on to take their own life.
It’s a startling fact. Most people I’ve trained, or spoken to, during my work with the Luna Foundation assume that young people bereaved as teenagers are at a greater risk. We’ve certainly seen situations where the focus is on supporting older bereaved children and really just ensuring the basic needs of the younger child are…
Highly commended in the Kent Mental Wellbeing Awards
I’m very pleased to report that Luna Foundation’s project in Kent and Medway has been highly commended in the Kent Mental Wellbeing Awards. The panel was ‘extremely impressed’ at the work Luna has delivered in Kent and Medway to improve the support for children and young people bereaved by suicide and ‘the amount of hard…
How To Help Someone After a Miscarriage reviewed in BJ Psych Bulletin
New review How to Help Someone After a Miscarriage has been reviewed in the British Journal of Psychiatry’s Bulletin. You can read the review here. Foster’s own difficult experience combined with her commitment to representing the views of the many women who have experienced miscarriage lends a personal and empathetic quality to the advice provided…….
Supporting children under five who lose a parent to suicide
Would you like to play a key role in improving support for young children bereaved by parental suicide? Losing a parent or carer to suicide during childhood can have a devastating and long-term impact on a young person’s mental health. Research has shown that children who are bereaved by parental suicide when aged between two…
Moderating Facebook groups – online training for Leukaemia Care volunteers
Last week I completed the second of two online training sessions for Leukaemia Care‘s new volunteer moderators. Like many organisations, their support group offering on Facebook had traditionally sat with their social media team. As their support groups have grown, so has the need for independent moderation and overview (I’ve written more about this here)….
Celebration and workshop with the Luna Lived Experience Network
Last week I was back in London for the first time since Covid lockdowns and baby Jay (who is now two and no longer really a baby). I was there to celebrate Luna Foundation’s first birthday at RSA House. The Luna Foundation Luna was established on 17 March 2022 by Anna Wardley. Anna’s father, Ralph,…
New website for Action on Postpartum Psychosis
Over 2022 I have been project-managing (and doing the majority of the work on) a new website for Action on Postpartum Psychosis (APP). APP is a small charity, struggling after Covid and with the cost of living crisis. They could not afford an expensive agency to work on their new design, structure and content. A…
Luna Foundation leaflets published
Leaflets for parents and professionals supporting children bereaved by parental suicide Before Christmas I wrote about Anna Wardley’s Four Thought about parental suicide and the work I am doing for the Luna Foundation. I’m now pleased to say the two new leaflets – one for families and one for professionals are now available on Luna’s…
Book your place on the new Miscarriage Association workplace training now
Open session taking place on March 1st The first of what I hope will be many of the new Miscarriage Association workplace training sessions are now available to book online here. These have been in development for a while now and are based on the research and resource development I did in 2019. Sessions to…